Understanding Disc Herniation: The Basics
What Is a Disc Herniation?
Your spine is made up of bones (vertebrae) separated by soft cushions called spinal discs. These discs act as shock absorbers and allow your spine to move smoothly. Each disc has a soft inner core and a tougher outer layer.
A disc herniation (often called a “slipped disc”) occurs when the inner portion pushes through a tear or weak spot in the outer layer. While the disc doesn’t literally slip out of place, the bulging material can press against nearby nerves and trigger symptoms.
How a Herniation Causes Symptoms
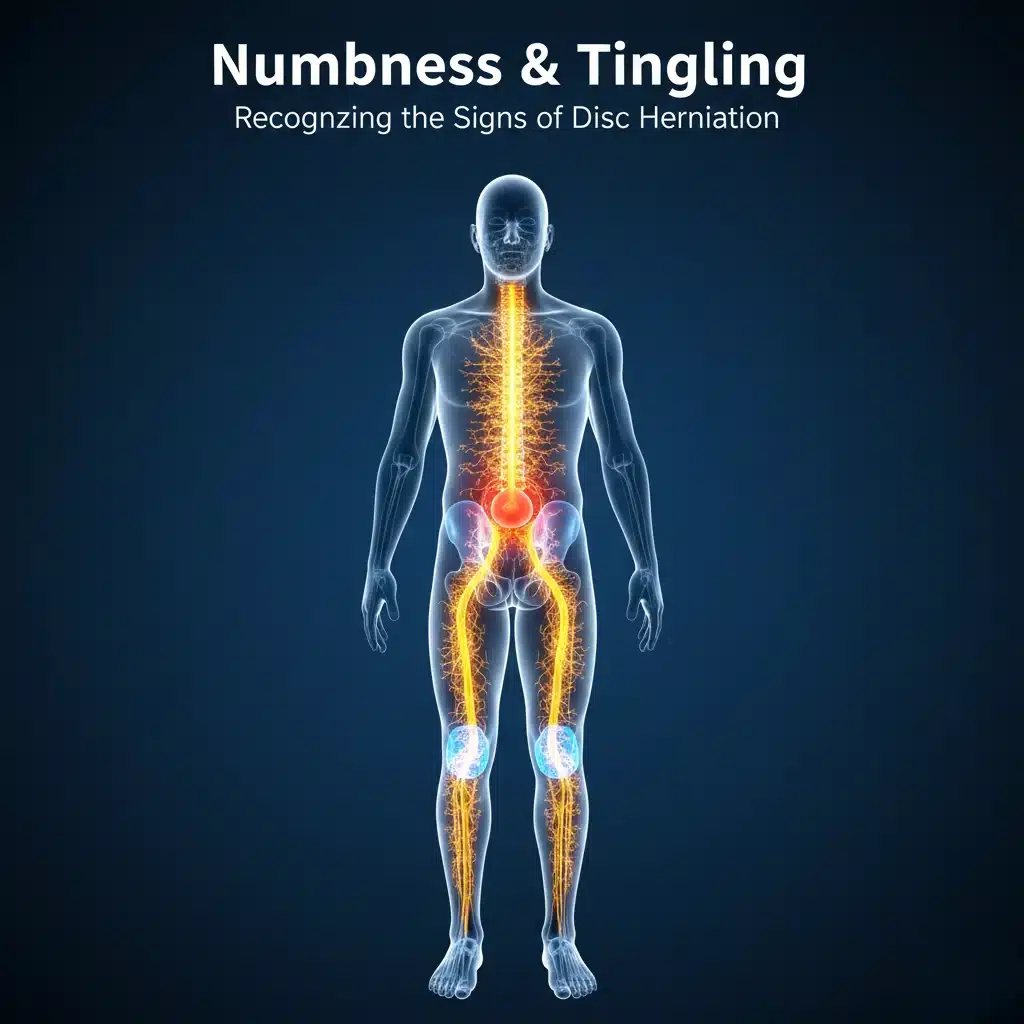
When disc material protrudes, it can irritate or compress spinal nerves. These nerves control sensation and muscle movement. Compression disrupts normal nerve signaling, which can lead to pain, tingling, numbness, or weakness in areas served by the affected nerve.
The Primary Warning Sign: Numbness and Tingling
Dermatomes and Nerve Root Compression
Your skin is mapped into regions called dermatomes, each supplied by a single spinal nerve. When a specific nerve root is compressed by a herniated disc, symptoms often appear in the dermatome associated with that nerve.
For example, nerve compression in the lower back may cause numbness or tingling down the leg, while compression in the neck can cause symptoms in the arm or hand. This pattern helps clinicians identify which nerve is involved.
Paresthesia: Tingling and the “Pins and Needles” Feeling
The tingling, buzzing, or “pins and needles” sensation is known as paresthesia. It is a common early sign of nerve irritation and may come and go at first. Paresthesia often appears with certain movements, prolonged sitting, or awkward postures.
True Numbness: A Red Flag
True numbness—a noticeable loss of sensation—can signal more severe nerve compression. If numbness is persistent, spreading, or accompanied by weakness, it’s important to seek professional evaluation. These changes suggest that nerve signaling may be significantly impaired.
Beyond Numbness: Other Key Disc Herniation Signs
Radiating Pain (Radiculopathy)
Radiculopathy refers to nerve pain that radiates away from the spine. It is often sharp, burning, or electric in nature.
- Cervical disc herniation can cause pain down the shoulder and arm.
- Lumbar disc herniation can cause pain into the buttock and leg.
Sciatica: The Most Common Lumbar Sign
Sciatica is radiating leg pain caused by irritation of the sciatic nerve, commonly due to a herniated disc in the lower back. Pain often follows a distinct path from the lower back through the buttock and down the leg.
Muscle Weakness
Compression of motor nerve fibers can cause muscle weakness, such as difficulty lifting the foot, climbing stairs, or gripping objects. Weakness is a more concerning sign than pain alone and should be medically assessed.
Changes in Reflexes
Nerve compression can alter reflexes. During an exam, clinicians may find reduced or absent reflexes in the affected limb, which helps determine the level and severity of nerve involvement.
When Numbness Signals an Emergency
Cauda Equina Syndrome (CES): Immediate Attention Required
Cauda Equina Syndrome (CES) occurs when a large disc herniation compresses the bundle of nerves at the base of the spinal cord. This is a medical emergency and requires immediate treatment to prevent permanent nerve damage.
Red Flag Symptoms of CES
Seek urgent medical care if you experience:
- Saddle anesthesia: numbness in the groin, inner thighs, or buttocks
- New-onset bowel or bladder dysfunction: difficulty urinating or incontinence
- Severe, progressive leg weakness
- Worsening numbness affecting both legs
Diagnosis and Next Steps
How a Doctor Confirms a Disc Herniation
Diagnosis may include:
- Review of medical history and symptoms
- Physical and neurological examination
- Imaging tests such as MRI to visualize disc and nerve involvement
Treatment Options
Treatment depends on symptom severity and may include:
- Activity modification and rest
- Anti-inflammatory or pain-relief medications
- Physical therapy and guided exercises
- Targeted injections to reduce nerve inflammation
- Surgical options for persistent pain or neurological deficits
Many people improve with conservative, non-surgical care.
Conclusion and Outlook
Numbness and tingling can be early signs of disc herniation and should not be ignored—especially when paired with radiating pain or weakness. The outlook is often positive with early evaluation and appropriate care. With the right treatment plan, many people experience symptom relief and return to normal activities.
Frequently Asked Questions (FAQ)
Is numbness always caused by a herniated disc?
No. While disc herniation is a common cause, numbness can also result from other conditions such as nerve entrapment, spinal stenosis, diabetes-related neuropathy, or circulation issues. A proper evaluation is needed to identify the exact cause.
Can numbness from a herniated disc go away on its own?
Yes, in many cases numbness improves as inflammation decreases and the disc heals over time. Conservative treatments such as rest, physical therapy, and posture correction can support recovery. Persistent or worsening numbness should be evaluated by a professional.
How long does numbness from a disc herniation last?
Symptoms vary from person to person. Some people experience improvement within weeks, while others may have lingering symptoms for months. Early intervention often leads to faster and more complete recovery.
When should I worry about numbness or tingling?
You should seek professional care if numbness is persistent, spreading, associated with weakness, or interfering with daily activities. Sudden numbness combined with bowel or bladder changes requires urgent medical attention.
Can chiropractic or physical therapy help with disc-related numbness?
Conservative care such as physical therapy or chiropractic management may help reduce nerve pressure, improve mobility, and support recovery in many cases. The best approach depends on your specific diagnosis and symptom severity.